Visit and Join the WeHeal Umbilical Cord Stem Cells (UCSCs)
For more information, see: MayoClinic | Wikipedia
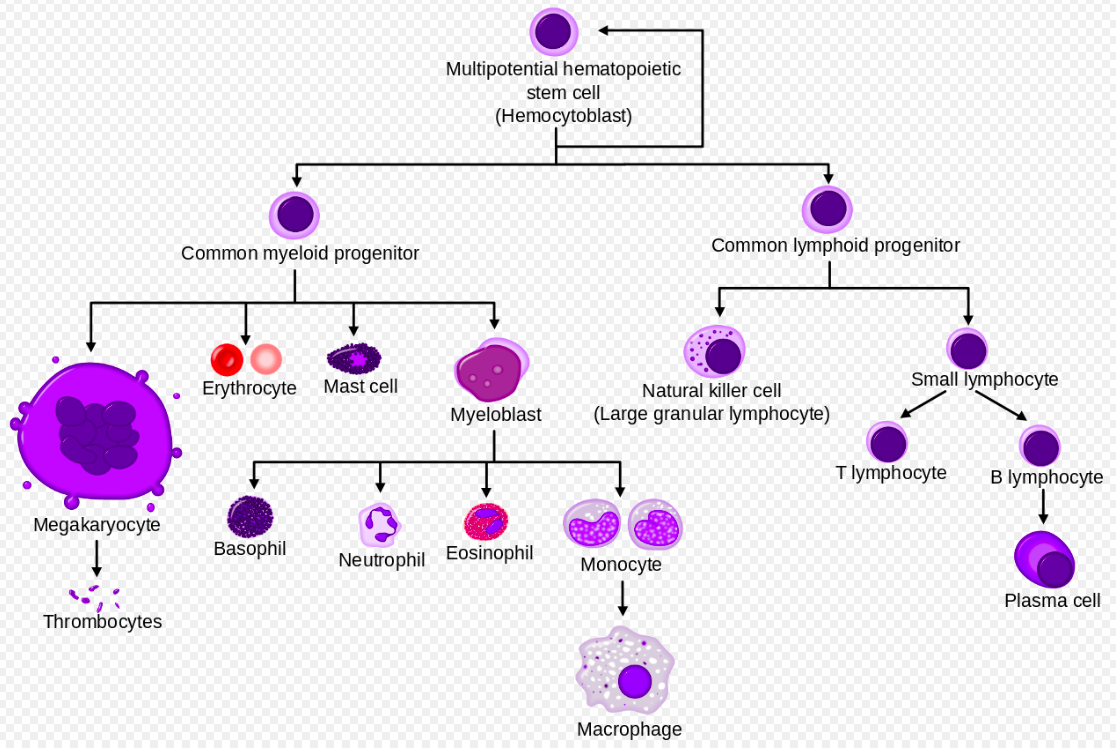
“NOTE: WeHeal.org founder Eric Drew was one of the first adults in the world to survive from a multiple umbilical cord stem cell transplant which was performed at Fairview Medical Center at Minnesota State University in Minneapolis, Minnesota. Please see “”Eric’s Story”” on “”Home Page”” for more information. Cord blood is a sample of blood taken from a newborn baby’s umbilical cord. It is a rich source of hematopoietic stem cells, which are precursors to blood cells. As such, they have been used to treat certain diseases of the blood and immune system. The next largest group is inherited diseases (of red blood cells, the immune system and certain metabolic abnormalities.) Patients with lymphoma, myelodysplasia and severe aplastic anemia have also been successfully transplanted with cord blood.[citation needed] Cord blood is collected from the umbilical cord vein attached to the placenta after the umbilical cord has been detached from the newborn.[1] Cord blood is collected because it contains stem cells, including hematopoietic cells, which can be used to treat hematopoietic and genetic disorders. One unit of cord blood generally lacks stem cells in a quantity sufficient to treat an adult patient. The placenta is a much better source of stem cells since it contains up to ten times more than cord blood.[2] Some placental blood may be returned to the neonatal circulation if the umbilical cord is not prematurely clamped.[3] According to Eileen K. Hutton, PhD, and Eman S. Hassan, MBBch, cord clamping should be delayed a minimum of two minutes to prevent anemia over the first three months of life and enriching iron stores and ferritin levels for as long as six months. (Ref. “”Late vs Early Clamping of the Umbilical Cord in Full-term Neonates,”” JAMA, March 21, 2007) If the umbilical cord is not clamped, and it is not during an extended-delayed cord clamping protocol, a physiological postnatal occlusion occurs upon interaction with cold air, when the internal gelatinous substance, called Wharton’s jelly, swells around the umbilical artery and veins.
Umbilical cord blood is the blood left over in the placenta and in the umbilical cord after the birth of the baby. The cord blood is composed of all the elements found in whole blood. It contains red blood cells, white blood cells, plasma, platelets and is also rich in hematopoietic stem cells. There are several methods for collecting cord blood. The method most commonly used in clinical practice is the “”closed technique””, which is similar to standard blood collection techniques. With this method, the technician cannulates the vein of the severed umbilical cord using a needle that is connected to a blood bag, and cord blood flows through the needle into the bag. On average, the closed technique enables collection of about 75 ml of cord blood.[4]
Collected cord blood is cryopreserved and then stored in a cord blood bank for future transplantation. A cord blood bank may be private (i.e. the blood is stored for and the costs paid by donor families) or public (i.e. stored and made available for use by unrelated donors). While public cord blood banking is widely supported, private cord banking is controversial in both the medical and parenting community. Although umbilical cord blood is well-recognized to be useful for treating hematopoietic and genetic disorders, some controversy surrounds the collection and storage of umbilical cord blood by private banks for the baby’s use.
Cord blood is stored by both public and private cord blood banks. Public cord blood banks store cord blood for the benefit of the general public, and most U.S. banks coordinate matching cord blood to patients through the National Marrow Donor Program (NMDP). Private cord blood banks are usually for-profit organizations that store cord blood for the exclusive use of the donor or donor’s relatives. Public cord blood banking is supported by the medical community. However, private cord blood banking is generally not recommended unless there is a family history of specific genetic diseases. New parents have the option of storing their newborn’s cord blood at a private cord blood bank or donating it to a public cord blood bank. The cost of private cord blood banking is approximately $2000 for collection and approximately $125 per year for storage, as of 2007. Donation to a public cord blood bank is not possible everywhere, but availability is increasing. Several local cord blood banks across the United States are now accepting donations from within their own states. The cord blood bank will not charge the donor for the donation; the OB/GYN may still charge a collection fee, although many OB/GYNs choose to donate their time. After the first sibling-donor cord blood transplant was performed in 1988, the National Institute of Health (NIH) awarded a grant to Dr. Pablo Rubinstein to develop the world’s first cord blood program at the New York Blood Center (NYBC),[6] in order to establish the inventory of non embryonal stem cell units necessary to provide unrelated, matched grafts for patients.
”
Visit and Join the WeHeal Umbilical Cord Stem Cells (UCSCs)
For more information, see: MayoClinic | Wikipedia
WeHeal is very grateful to our valued sources of information which include Wikipedia, WebMD, ClinicalTrials.gov, Cancer.gov, Infoplease, and the US CDC (Center for Disease Control).